Hey there! If you’ve ever been to a hospital or clinic, you’ve probably been amazed (or frustrated) at how the healthcare system juggles countless patient records. From diagnoses to treatments, lab results, and prescriptions, the amount of data that every patient’s medical chart brings is colossal. But have you ever paused and wondered, how do healthcare professionals manage it all? Where do these records go, and how are they accessed whenever required?
Enter the realm of electronic medical record software.
Now, if you’re envisioning a basic digital folder where your patient medical records are thrown in, think bigger and smarter. In our rapidly digitizing world, medical record software, also known as Electronic Health Records (EHR) or Electronic Medical Records (EMR), is the backbone of modern healthcare data management. These systems don’t just ‘store’ information; they make it accessible, actionable, and secure.
Think of it this way: remember the last time you had to rummage through a stack of papers to find that one important document? Now imagine doing that for thousands of patients daily. Sounds daunting, right? With medical record software, that exhausting rummage transforms into a few simple clicks. It’s like having a super-organized, always-available digital assistant specifically for patient charts and data.
But it’s not just about convenience. The implications of this medical software suite extend far and wide, ensuring patient privacy, better treatment decisions, efficient communication among medical professionals, and much more.
In this comprehensive blog post, we will embark on a journey, unraveling the mysteries of medical record software. We’ll delve deep into its components, its significance in enhancing healthcare services, its transformative impact on patient care, and why every modern healthcare facility needs to jump on this bandwagon.
So, whether you’re a curious patient’s medical history, a healthcare professional looking to update your clinic’s operations, or just someone fascinated by healthcare tech, stick around. This is going to be a fascinating exploration!
Medical record software is a digital platform for human services organizations to streamline patient data management. It not only enhances healthcare services but also aids healthcare organizations in ensuring patient privacy and efficient communication among medical professionals.

What is Medical Record Software?
At its core, medical record software serves as the digital brain of large healthcare organizations and institutions. But what exactly does it do? Let’s dive into the nitty-gritty of it.
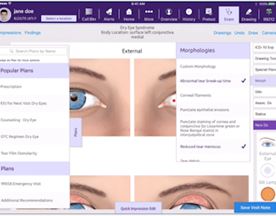
Medical record software, popularly referred to as Electronic Health Records software (EHR) or as Electronic Medical Records software (EMR), is essentially a computerized version of a patient’s paper chart. However, comparing it to a mere digitalized paper chart would be an understatement. This software isn’t just a direct digital translation of paper files; it’s an intelligent, interconnected, and dynamic system that captures, stores, and retrieves patient data in real-time. It’s the unsung hero that ensures medical professionals always have a comprehensive overview of a patient’s health at their fingertips.
In-Depth Components of Electronic Medical Record (EMR) Software:
- Patient Data: This encompasses the patient’s personal information like name, date of birth, address, and contact details. Additionally, it stores a patient’s entire medical history, previous diagnoses, treatment plans, allergies, immunization dates, radiology images, and outcomes of past treatments.
- Billing Information: Beyond clinical data, medical record software seamlessly integrates the financial aspect of healthcare. It manages and automates the billing process, ensuring that payment details, insurance information, and treatment costs are accurately recorded and processed.
- Prescription and Medication Records: One of the significant challenges in healthcare is ensuring that prescriptions are accurate and that medication errors are minimized. This software ensures that every drug prescribed is documented, allowing for a review of potential interactions or allergies. It also aids pharmacists in verifying and dispensing medications accurately.
- Lab Results: Waiting for lab results can be a nerve-wracking experience for patients. Medical record software bridges the communication gap between labs and doctors. It integrates seamlessly with various lab systems, ensuring timely and efficient delivery of results directly to the concerned healthcare provider. This not only expedites diagnosis and treatment but also reduces the chances of manual errors.
- Interoperability: One of the most remarkable features of modern EHR systems is their ability to “talk” to other systems. This means that a patient’s data isn’t siloed within one institution. If a patient goes to a specialist or needs emergency care at another hospital, their medical data can be easily accessed, given the right permissions.
- Real-Time Updates: The dynamic nature of this software means that any changes, additions, or updates to a patient’s record are reflected in real-time. This is crucial for healthcare professionals making on-the-spot decisions based on the most current data.
Summary:
- Medical record software is a comprehensive and interconnected system that captures, stores, and retrieves patient data.
- It combines clinical, financial, and administrative data into a unified platform.
- Features like interoperability and real-time updates make it indispensable in modern healthcare settings.
The Benefits of Using Medical Record Software
In today’s rapidly changing healthcare landscape, staying efficient, responsive, and patient-centered is more crucial than ever. And here’s the thing: medical record software plays a pivotal role in ensuring just that. Let’s delve deeper into why this software isn’t just a convenience but a game-changer for healthcare institutions and professionals.
1. Efficiency and Streamlined Workflows
Before the advent of EHRs, healthcare professionals were entangled in a web of paperwork. Every appointment, prescription, test, and diagnosis resulted in multiple pages added to a patient’s file. Medical record software effectively dismantles this bureaucratic hurdle.
- Quick Access to Patient History: No more thumbing through thick files. With a few clicks, a doctor can access a patient’s complete medical history, helping them make informed decisions faster.
- Reduced Administrative Overhead: By digitizing records and automating repetitive tasks, healthcare institutions can reallocate resources more efficiently, ensuring staff can focus on patient care rather than paperwork.
2. Enhanced Data Accessibility
The seamless flow of information is crucial in healthcare. With medical record software:
- Anytime, Anywhere Access: Authorized professionals can access the necessary patient data from different departments or even different locations, aiding in coordinated and timely care.
- Collaboration: Different specialists treating the same patient can effortlessly collaborate, ensuring a more holistic approach to patient care.
3. Elevated Quality of Patient Care
When doctors have comprehensive information about behavioral and mental health,, at their disposal, they’re better equipped to diagnose, treat, and care for their patients.
- Informed Decision Making: Having a patient’s complete health history, including past ailments, allergies, and medications, ensures that doctors make well-informed decisions that consider all potential risks and benefits.
- Patient Engagement: Many medical record software solutions come with patient portals, enabling patients to access their health data, understand their treatments better, and engage proactively in their healthcare journey.
4. Robust Data Security and Compliance
While digitization brings forth concerns about data security, EHRs are typically built with robust security measures.
- Advanced Encryption: These systems utilize advanced encryption techniques, making unauthorized access extremely difficult.
- Regulatory Compliance: With increasing regulations around patient data protection, medical record software ensures compliance with standards, protecting both the patient and the institution from potential legal complications.
5. Cost-Effectiveness
While the initial investment in medical record software might seem steep, the long-term financial benefits are undeniable.
- Reduction in Errors: Digital systems significantly reduce manual errors in prescriptions, billing, and patient records, which can otherwise lead to expensive lawsuits or re-treatments.
- Operational Efficiency: With streamlined workflows, institutions can operate more efficiently, leading to potential cost savings in administrative tasks.
Summary:
- Medical record software drastically improves efficiency, reducing the time spent on administrative tasks and paperwork.
- It facilitates better decision-making by providing comprehensive patient data to healthcare professionals in real-time.
- Enhanced data security and compliance with regulatory standards protect both patients and institutions.
- Despite initial costs, the software proves cost-effective in the long run by improving operational efficiency and reducing errors.

Software Tools to Consider
In the realm of medical record software, there’s no one-size-fits-all. Depending on the size of medical practice management the healthcare institution, their specific needs, and budget, different solutions might be more appropriate. However, if you’re just venturing into this territory or looking to upgrade practice management solution, here are some top software tools in the industry that have been receiving raving reviews from healthcare professionals.
Epic Systems Corporation
- Overview: A leader in the EHR industry, Epic Systems offers a wide range of health software solutions. Known for its comprehensive platform and interoperability, it’s especially favored by large hospitals and health systems.
- Features: Integration with specialty-specific systems, a patient portal, and robust data analytics tools.
Cerner Millennium
- Overview: Cerner’s Millennium software is another heavyweight in the world of EHR. It’s designed to provide a unified EHR system across all healthcare environments – from private practices to large hospitals.
- Features: Real-time patient data access, revenue cycle management capabilities, and a patient portal for more dynamic engagement.
Allscripts Professional EHR
- Overview: Tailored more for smaller to mid-sized healthcare practices, Allscripts offers an intuitive user interface combined with a powerful set of tools.
- Features: Integrated practice management features, mobile patient portal, and extensive e-prescribing capabilities.
Athenahealth
- Overview: Known for its cloud-based deployment, Athenahealth is a favorite among small to medium-sized practices looking for flexibility and scalability.
- Features: Integrated billing system, patient engagement tools, and a dashboard for real-time performance insights.
Meditech EHR
- Overview: An integrated EHR solution that caters to a wide range of healthcare environments, from critical access hospitals to entire healthcare networks.
- Features: Interdisciplinary patient care tools, financial and administrative tools, and a web-based patient and consumer health portal.
Why These Tools Stand Out
- Customizability: While standard features are essential, the best EHR systems offer a degree of customizability, allowing institutions to tailor the software to their specific needs.
- User Experience: Intuitive interfaces, easy navigation, and accessibility contribute to why these tools are preferred by many professionals. After all, the last thing a doctor wants is to wrestle with software during a busy day.
- Training and Support: These companies not only provide robust software solutions but also ensure ongoing training and support, helping institutions make the most of their investment.
Summary:
- Epic Systems and Cerner Millennium cater especially to larger healthcare institutions, offering comprehensive and integrated EHR solutions.
- Allscripts, Athenahealth, and Meditech provide versatile solutions suitable for varying sizes of healthcare practices.
- Factors like customizability, user experience, and ongoing support make these tools stand out in the crowded market.
FAQs on Medical Record Software
Medical record software, with its technical nuances and vast implications for patient care, often gives rise to numerous questions. Here, we tackle some of the most frequently asked questions to shed light on this indispensable tool.
1. What’s the difference between EMR and EHR?
While often used interchangeably, there’s a subtle distinction:
- EMR (Electronic Medical Records): These are digital versions of the paper charts in the clinician’s office. They contain the medical and treatment history of patients in one practice.
- EHR (Electronic Health Records): EHRs go beyond the data collected in a provider’s office and include a more comprehensive patient history. They’re designed to be shared with other providers, thus providing a broader view of a patient’s care.
2. How secure is the patient data in EHR systems?
Medical record software is designed with robust security measures, including:
- Advanced encryption techniques.
- Multi-factor authentication.
- Regular security audits. Most EHR vendors also ensure compliance with health information privacy laws, further safeguarding patient data.
3. Can patients access their own health records?
Absolutely! Many EHR systems come with patient portals that allow individuals to view their medical histories, test results, and even upcoming appointments. This fosters a proactive approach to personal health.
4. How do EHRs improve patient care?
EHRs contribute to enhanced patient care by:
- Providing real-time, comprehensive patient data to healthcare providers.
- Reducing the chances of medication errors.
- Streamlining administrative tasks, allowing more focus on patient care.
5. What about interoperability? Can EHRs communicate with other systems?
Yes, modern EHRs emphasize interoperability, enabling these systems to share and synchronize patient data across various other healthcare facilities and settings – be it labs, other health care providers, hospitals, or specialists.
6. Are there any downsides to using medical record software?
While the benefits outweigh the drawbacks, some challenges include:
- Initial high costs of setup and training.
- Resistance from staff in adapting to new technologies.
- Potential software glitches.
7. How do EHRs handle data backups?
Most EHRs integrate automatic backup systems that store data redundantly in multiple secure locations. This ensures data recovery in case of any unforeseen events like power failures or system crashes.
8. Can EHRs integrate with billing systems?
Indeed, many EHR systems come with integrated practice management software tools, streamlining billing processes, handling insurance claims, and medical billing software ensuring a seamless financial workflow.
9. Is the transition from paper records to EHRs challenging?
Transitioning involves a learning curve. However, with proper training, support from the EHR software vendor, and a gradual, phased approach, the transition can be smoother than anticipated.
10. How do medical record software solutions stay updated with medical advancements?
Top: EHR software vendors regularly update their software, ensuring that they integrate the latest medical guidelines, research findings, and regulatory changes. These updates help in keeping the software current and relevant to evolving healthcare needs.
Summary:
- EMR and EHR have distinct differences, primarily in scope and shareability.
- EHR systems prioritize robust security measures to safeguard patient data.
- Modern EHRs focus on interoperability, enhancing comprehensive patient care.
- While challenges exist, the benefits of EHRs in streamlining healthcare processes and improving patient outcomes are undeniable.

Historical Context: The Evolution of Medical Record Keeping
Medical record keeping has been an indispensable aspect of healthcare for millennia. A deep dive into its history reveals not only the journey of medicine but also mirrors the evolution of human civilization, technology, and communication methods.
Stone Tablets to Papyrus Scrolls: The Beginnings
Long before the digital age, ancient civilizations understood the importance of recording their medical practices and observations. These records often intertwined with religious practices, magic, and early medicinal theories.
- Ancient Mesopotamia: Here, cuneiform inscriptions on clay tablets provide the earliest examples of medical record keeping. These tablets, some dated as far back as 2100 BC, recorded symptoms, diagnoses, and treatments. They offer insights into early surgical practices and the medicinal properties of various herbs.
- Ancient Egypt: Papyrus scrolls, such as the renowned Edwin Smith Papyrus and Ebers Papyrus, provide detailed accounts of surgical procedures, anatomical observations, and disease treatments. These documents, dating around 1600 BC, highlight the ancient Egyptians’ surprisingly advanced grasp of human anatomy and their methodical approach to medicine.
Middle Ages to Renaissance: Monastic Records to Medical Manuscripts
The fall of the Roman Empire and the onset of the Dark Ages saw a shift in medical practice and record keeping. Monasteries became the primary centers of learning and healing.
- Monastic Records: Monasteries across Europe maintained infirmaries to care for the sick. Monks, as the primary caregivers, maintained meticulous records of patients’ symptoms, treatments, and outcomes, often integrating spiritual remedies alongside herbal treatments.
- Medical Manuscripts: The Renaissance period ushered in a renewed interest in science and medicine. Medical students and doctors began to compile manuscripts, detailing observations, dissecting human bodies, and recording findings. The works of luminaries like Avicenna and Hippocrates were translated and widely disseminated.
20th Century: The Age of Paper and Files
The turn of the 20th century brought about significant advancements in medicine and administrative practices. With increasing patient numbers and the evolution of hospitals into complex institutions, a systematic method of doing medical billing and keeping patient records became paramount.
- Paper-Based Records: By the mid-20th century, the ubiquitous patient file had become an essential part of any doctor’s office. Stored in vast filing cabinets, these records tracked a patient’s history, from consultation notes to test results.
- The Initial Digital Shift: By the late 20th century, with the rise of computers, some forward-thinking institutions began to see the value in digital record-keeping. These rudimentary systems, though limited, marked the beginning of a transformative era in medical record keeping.
Into the Digital Age: EHRs and Beyond
The transition into the 21st century accelerated the shift behavioral health practices from paper to pixels. The development of more advanced computing capabilities, coupled with the need for streamlined, accessible patient information, led to the rapid evolution and adoption of Electronic Health Records (EHRs). While these systems initially faced resistance due to their perceived complexity and high costs, the undeniable benefits they brought in terms of accessibility, accuracy, and efficiency soon made them the gold standard in healthcare institutions worldwide.
Summary:
- Medical record keeping has evolved from inscriptions on stone tablets in ancient civilizations to sophisticated digital systems today.
- Each era brought its unique medium, from papyrus scrolls to paper files, and finally to digital screens.
- The journey of medical record keeping reflects the broader trajectory of human advancement, weaving together threads of history, culture, technology, and medicine.

Key Features to Look for in Medical Record Software
Choosing an EHR (Electronic Health Record) system for a healthcare institution is no small feat. With the proliferation of numerous software options in the cloud based software market, it can feel daunting to pick the right one. However, a deep understanding of the essential features that make an EHR truly effective can guide this decision-making process.
1. User-Friendly Interface
- Importance: EHRs are used daily by healthcare professionals, many of whom may not be tech-savvy. An intuitive interface ensures that they can navigate the system with ease, without the stress of a steep learning curve.
- Look for: Simple navigation menus, clear icons, and a layout that resembles familiar software. Some EHRs also offer customizable dashboards, allowing users to tailor the system to their specific needs.
2. Customization
- Importance: Healthcare is multifaceted. What works for a general practitioner might not work for a specialist or a large hospital. The software should be adaptable to various settings and workflows.
- Look for: Modules that can be added or removed based on the institution’s needs. For instance, a dermatologist might benefit from a visual body map tool, while a pediatrician might need growth chart tracking.
3. Mobile Access
- Importance: With doctors and healthcare professionals constantly on the move between consultations, wards, and even multiple clinics, having access to patient records on-the-go is crucial.
- Look for: EHRs that offer a mobile version or app that is compatible with both iOS and Android devices. This app should maintain the primary functionalities of the desktop version but optimized for a mobile screen. Features like offline access can be a bonus, especially in areas with connectivity issues.
4. Integrated Billing
- Importance: Merging patient care with billing not only streamlines administrative tasks but also reduces billing errors, ensuring that healthcare institutions maintain financial health.
- Look for: An EHR system that can generate bills based on the services rendered, keeping track of insurance details, co-pays, and outstanding balances. Integration with popular payment gateways or platforms can also be beneficial.
5. Interoperability
- Importance: Healthcare is collaborative. Professionals from various disciplines often need to work together. An EHR system should allow seamless sharing of patient data between departments or even different institutions.
- Look for: EHR systems that adhere to interoperability standards, allowing them to communicate with other systems easily. The capability to export patient summaries in universally readable formats is a plus.
6. Enhanced Security Features
- Importance: Patient records are sensitive. With rising cyber threats, it’s paramount that the EHR system safeguards this information.
- Look for: Encryption protocols, multi-factor authentication, and regular software updates. Some EHRs also offer audit trails, which track every access and change made to a patient’s record.
7. Cloud-Based vs. On-Premises
- Importance: Deciding between a cloud-based system and an on-premises one depends on the institution’s infrastructure, budget, and tech capabilities.
- Look for: If opting for a cloud-based system, ensure the service provider has reliable uptime and robust data backup mechanisms. On-premises systems, while potentially more secure, might entail higher initial setup costs and IT maintenance.
8. Reporting and Analytics
- Importance: Beyond daily patient care, EHRs can offer insights into broader healthcare trends, patient demographics, and more, assisting in research and administrative decision-making.
- Look for: Features that allow the generation of customizable reports, charts, and graphs. A good EHR might also offer predictive analytics, helping institutions anticipate future trends or challenges.
Summary:
- Selecting the right EHR requires a keen understanding of both the institution’s specific needs and the essential features that an effective EHR should possess.
- User experience, customization, mobility, integrated billing, interoperability, security, deployment model, and analytics capabilities stand out as some of the pivotal features to consider.
- While features are paramount, it’s also crucial to consider post-purchase support, training, and the vendor’s reputation in the industry.

The Role of Artificial Intelligence in EHRs
In the modern digital landscape, where technology continues to revolutionize industries at a breakneck pace, healthcare is no exception. Among the most potent catalysts of this transformation is Artificial Intelligence (AI). When integrated with Electronic Health Records (EHRs), AI promises not just to enhance the user experience but to fundamentally reshape patient care.
1. Predictive Analytics for Improved Patient Outcomes
- Importance: AI can sift through vast amounts of data in EHRs to detect patterns that might not be immediately visible to healthcare professionals.
- Implementation: By analyzing a patient’s history, current health status, and millions of other records, AI can predict potential health risks or complications. For instance, AI could anticipate a patient’s likelihood of readmission or flag potential allergic reactions based on medication interactions and the patient’s past records.
2. Streamlining Administrative Tasks
- Importance: Physicians often report that EHR-related tasks, such as data entry, take up a significant portion of their time, diverting them from patient care.
- Implementation: Natural Language Processing (NLP), a subset of AI, can convert a doctor’s voice notes into structured EHR entries. Furthermore, AI algorithms can auto-populate fields based on context, reducing manual entry requirements.
3. Enhanced Diagnostic Accuracy
- Importance: Even the most seasoned professionals can occasionally overlook details. AI offers an additional layer of analysis, ensuring that nothing is missed.
- Implementation: By analyzing imaging results, blood test reports, and patient symptoms, AI can assist doctors in making more accurate diagnoses. For instance, in radiology, AI systems can highlight abnormalities in X-rays or MRIs that could be indicative of diseases like cancer.
4. Personalized Treatment Plans
- Importance: Every patient is unique, and a one-size-fits-all approach is often not optimal.
- Implementation: AI can analyze a patient’s genetic makeup, health history, and current condition to suggest tailored treatment plans. This can be particularly impactful in fields like oncology, where personalized treatment can mean the difference between recovery and relapse.
5. Improved Follow-Up and Patient Engagement
- Importance: Ensuring patients adhere to treatment plans and attend follow-up appointments is crucial for positive health outcomes.
- Implementation: AI-driven chatbots and virtual assistants can send reminders to patients, answer their queries 24/7, and even monitor treatment compliance through wearable integrations.
6. Research and Drug Discovery
- Importance: The vast amounts of data in EHRs can be invaluable for medical research.
- Implementation: AI can analyze these massive datasets to identify potential trends, correlations, and insights, accelerating drug discovery and the development of novel treatment methods.
7. Enhancing Telemedicine
- Importance: With the increasing adoption of telehealth, especially post the COVID-19 pandemic, providing quality care remotely has become paramount.
- Implementation: AI can assist healthcare professionals during teleconsultations by quickly pulling up relevant patient data, suggesting potential diagnoses based on the symptoms described, and even monitoring patients in real-time through connected devices.
Summary:
- AI’s integration with EHRs is not merely a futuristic concept; it’s rapidly becoming a present-day reality. Its potential to enhance patient care, improve healthcare outcomes, and streamline administrative tasks is undeniable.
- While AI offers many advantages, it’s essential to approach its integration ethically, ensuring patient data privacy and addressing potential biases in AI algorithms.
- As the symbiosis between AI and EHRs continues to mature, the overarching goal remains clear: harnessing technology to deliver better, more efficient, and personalized healthcare to all.

Global Perspectives: How Different Countries Are Adopting EHRs
Electronic Health Records (EHRs) are transforming healthcare around the world. While the core objective—digitizing patient health records—remains consistent globally, the journey of adoption, implementation, and innovation varies significantly across countries. Understanding these global perspectives can offer valuable insights into the multifaceted evolution of EHRs and their implications for future healthcare systems.
1. United States
- Adoption Overview: The US has made significant strides in EHR adoption, especially after the 2009 Health Information Technology for Economic and Clinical Health (HITECH) Act. This act provided financial incentives for healthcare providers to adopt and use EHRs.
- Unique Challenges: Interoperability between various EHR systems, concerns over patient data privacy, and a fragmented healthcare system have been notable challenges.
- Innovative Features: The integration of AI, telehealth functionalities, and patient portals for self-service are areas of ongoing innovation in the US EHR landscape.
2. United Kingdom
- Adoption Overview: The National Health Service (NHS) has embarked on ambitious plans over the years to implement EHR systems across its vast network of hospitals and clinics.
- Unique Challenges: Initial large-scale projects like the NHS’s National Programme for IT faced issues of overspending and delays. However, recent strategies emphasize a more decentralized approach to EHR adoption.
- Innovative Features: There’s a growing emphasis on creating unified patient records that can be accessed across different NHS entities, enhancing continuity of care.
3. Australia
- Adoption Overview: Australia’s approach to EHRs materialized as the My Health Record system, an opt-out digital health record platform for all citizens.
- Unique Challenges: Public concerns over data privacy and security were significant, leading to an opt-out period where citizens could choose not to have a digital health record.
- Innovative Features: My Health Record allows patients to view their health information, share it with various healthcare providers, and even add personal notes or advanced care directives.
4. Singapore
- Adoption Overview: Singapore’s National Electronic Health Record (NEHR) system aims to create a single health record for every citizen, accessible to all healthcare providers.
- Unique Challenges: Balancing the rapid technological advancements with a patient-centric approach to ensure that the system remains user-friendly for both healthcare providers and patients.
- Innovative Features: Integration of smart nation initiatives, including wearable technology data and telehealth, into the EHR system.
5. Canada
- Adoption Overview: Canada’s journey with EHRs is characterized by a collaborative approach, with provinces and territories spearheading initiatives tailored to their specific populations.
- Unique Challenges: Ensuring consistency and interoperability across the diverse EHR initiatives of different provinces and territories.
- Innovative Features: Emphasis on telehealth and remote patient monitoring, especially for remote and indigenous communities.
6. Scandinavia (Norway, Sweden, Denmark)
- Adoption Overview: Scandinavian countries, known for their robust healthcare systems, have been pioneers in EHR adoption, with almost universal coverage.
- Unique Challenges: As early adopters, these countries now face the challenge of updating and modernizing legacy systems.
- Innovative Features: High patient engagement with digital tools, seamless integration of health data from various sources, and advanced population health analytics.
Summary:
- The journey of EHR adoption, while rooted in the shared goal of digitizing health records, has unique pathways, challenges, and innovations across different countries. Factors such as government policies, cultural attitudes towards technology, healthcare infrastructure, and funding play significant roles in shaping these journeys.
- Lessons from these global perspectives underscore the importance of adaptability, patient-centricity, and continuous innovation in the realm of EHRs. They also highlight the need for international collaboration to share best practices and collectively advance the global healthcare landscape.
- As countries continue to evolve their EHR systems, the overarching vision is clear: leveraging technology to provide better healthcare outcomes, reduce costs, and enhance the patient experience.

Future Projections: The Next Step for Medical Record Software
The realm of medical record software is a landscape in flux, with technological, regulatory, and user-experience factors driving its evolution. As the adoption of Electronic Health Records (EHRs) becomes nearly universal in many parts of the world, the question arises: what’s next? Exploring the potential pathways for the future of medical record software offers a tantalizing glimpse into the transformative possibilities for global healthcare.
1. Hyper-Personalized Care Through Advanced Analytics
- Overview: The convergence of EHRs and advanced analytics, including AI, will allow for healthcare that’s tailored to individual patient profiles in unprecedented detail.
- Potential Impact: By analyzing a patient’s genetic, environmental, lifestyle, and clinical data, medical professionals can predict susceptibilities, tailor treatments, and even anticipate disease progression. Imagine a scenario where treatment recommendations are so personalized that they account for genetic markers, ensuring the highest efficacy and least side effects.
2. Seamless Integration with Wearable Technology
- Overview: The proliferation of wearable health tech—from smartwatches monitoring heart rates to specialized devices tracking blood sugar levels—will necessitate a tighter integration with EHRs.
- Potential Impact: Continuous real-time data from wearables can be integrated into patient records, offering a dynamic view of a patient’s health and potentially flagging abnormalities in real-time. This could revolutionize fields like remote patient monitoring, making healthcare more proactive rather than reactive.
3. Enhanced Voice Recognition and Interaction
- Overview: As voice recognition technology matures, its integration into EHR systems will become more sophisticated.
- Potential Impact: Medical professionals can interact with EHR systems hands-free, inputting patient data, querying records, or even receiving treatment suggestions using voice commands. This not only streamlines the data-entry process but also reduces potential errors, enhancing overall patient care.
4. Global EHR Interoperability
- Overview: With the push towards a globalized world, there’s an increasing need for EHR systems to be interoperable across borders.
- Potential Impact: A traveler from Australia needing medical attention in Canada can have their complete medical history accessible to the attending physician. This could dramatically improve the quality of emergency care for international patients and facilitate international medical collaboration.
5. Enhanced Cybersecurity Protocols
- Overview: As EHRs become more interconnected and sophisticated, they also become potential targets for cyber threats.
- Potential Impact: The future will likely witness a rise in advanced cybersecurity measures tailored for EHRs, ensuring patient data remains confidential and secure. Technologies like blockchain might play a role in enhancing data security and integrity.
6. Virtual and Augmented Reality in EHRs
- Overview: The integration of Virtual Reality (VR) and Augmented Reality (AR) technologies into EHR systems can revolutionize patient-doctor interactions.
- Potential Impact: Medical professionals could use AR to project layered patient data during consultations or even surgeries. Similarly, VR could be used for patient education, where they can ‘experience’ their medical conditions and understand treatment procedures in an immersive environment.
Summary:
- The future of medical record software isn’t just about incremental improvements but transformative shifts that could redefine the very essence of healthcare delivery.
- These projections are underpinned by technological advancements, but their success also hinges on user adoption, regulatory adaptations, and ensuring ethical considerations, especially in areas like patient data privacy.
- As medical record software evolves, it’s clear that the boundaries between technology and healthcare will continue to blur, ushering in an era of healthcare that’s more efficient, personalized, and patient-centric than ever before.

Conclusion
Stepping back and observing the vast landscape of healthcare, it becomes evident just how integral medical record software has become. From the bustling corridors of large hospitals to the quiet consultation rooms of private clinics, EHR systems have weaved themselves into the very fabric of modern medicine. And it’s not by mere chance.
The transition from paper-based systems to digital records has been a revolution in patient care. Gone are the days of misplaced papers, deciphering indecipherable handwriting, and long wait times due to administrative backlogs. In their place, we find instant data retrieval, seamless interdisciplinary collaborations, and empowered patients actively participating in their healthcare journeys.
However, it’s not just about the flashy digital interfaces or the convenience of clicking over writing. It’s about the tangible impact on healthcare outcomes. With EHRs, doctors are making better-informed decisions, institutions are reducing overheads and errors, and patients are receiving a quality of care previously unattainable.
Of course, challenges persist. Implementations are often costly, and technological hiccups can occur. However, as we’ve seen with the software tools explored and the myriad of benefits discussed, the advantages of medical record software are undeniable. The future of healthcare is digital, interconnected, and patient-centered, and EHRs are leading the charge.
In closing, whether you’re a healthcare professional exploring new medical software and options or a patient curious about the system safeguarding your medical history, understanding the world of EHRs is essential. Because, at the heart of it all, it’s not just about the medical software — it’s about healthier, happier lives.