Are you trying to figure out the difference between EHR vs EMR? Well, you’re in the right place. I’m here to break it down for you in a way that’s easy to understand and, hopefully, a bit fun too.
The Digital Revolution in Healthcare
Imagine you’re at the doctor’s office for a check-up. The doctor pulls up your medical history on a screen with just a few clicks. That’s the power of digital health records – they’ve revolutionized other health care providers and how we manage healthcare information.
But here’s the twist: not all digital records of a patient’s medical history and information are created equal. That’s where EHR (Electronic Health Records) and EMR (Electronic Medical Records) come into play.
The Origins of EHR and EMR
These terms might sound interchangeable, but there are a few key differences here. To understand them better, let’s take a quick trip down memory lane. It all started with EMRs, the first step in digitizing a patient’s care records. Think of EMRs as the digital version of your doctor’s old paper charts. They contain complete records of your medical and treatment history from one practice.
Then came EHRs. They’re like EMRs on steroids. EHRs are more comprehensive and are designed to be shared across different, healthcare organizations multiple providers and settings. This means that your patient’s EHR now contains a broader view of your health by including information from all the clinicians involved in your care.
EHR vs EMR: The Big Picture
Now, let’s zoom out for a second. The shift from EMR to EHR represents a fundamental change in the approach to managing a patient’s data information. It’s not just about electronic prescribing or going paperless. It’s about how healthcare professionals collaborate to manage patient data and how patients access their own health information.
The Impact of EHR and EMR on Healthcare
This change has huge implications. For healthcare providers, it’s about efficiency, accuracy, and coordination. For patients, it’s about empowerment and engagement in their own health. And for the healthcare system as a whole, it’s about improving health outcomes and reducing costs.
Key Points:
- EHRs and EMRs are different types of digital health records.
- EMRs are digital versions of paper charts in a single practice.
- EHRs provide a comprehensive, shared view of a patient’s health history.
- The shift from EMR to EHR has significant implications for healthcare delivery and patient empowerment.

EHR vs EMR: Understanding the Differences
Functionality and Scope
- EMR: Think of EMRs as a digital version of a patient’s chart. They’re used mainly by providers for diagnosis and treatment within a single practice.
- EHR: EHRs, on the other hand, are a more holistic view of a patient’s health. They can be shared across different healthcare settings, including labs, specialists, imaging facilities, pharmacies, emergency facilities, and school and workplace clinics.
Data Sharing and Accessibility
- EMR: EMRs are not built to be shared outside the individual practice. They’re great for tracking data over time, identifying patients due for checkups, and monitoring how patients measure up to certain parameters, like vaccinations and blood pressure readings.
- EHR: EHRs are designed to be accessed and shared. This sharing can improve the coordination of care and reduce medical errors, making the information available whenever and wherever it is needed.
Patient Involvement
- EMR: EMRs don’t typically provide patients with access to their own records. Interaction is limited mainly to the healthcare provider.
- EHR: EHRs often come with patient portals, which allow patients to easily access their health records, book appointments, request prescription refills, and communicate with their healthcare providers.
Legal and Compliance Aspects
- EMR: Since EMRs are contained within a single practice, they might not be subject to certain federal mandates that require the sharing of health information.
- EHR: EHRs, being more comprehensive and interconnected, are often designed to comply with national standards for data sharing, privacy, and security.
Key Points:
- EMRs are limited in functionality and scope compared to EHRs.
- EHRs facilitate greater data sharing and accessibility across various healthcare settings.
- EHRs offer more opportunities for patient involvement through patient portals.
- EHRs are typically designed to meet broader legal and compliance standards.

The Benefits of EHR Over EMR
Improved Patient Care
EHRs provide medical professionals with a more comprehensive view of a patient’s health, allowing for better-coordinated and more effective care. They also reduce the chances of medical errors.
Enhanced Data Security and Privacy
With EHRs, there’s a big emphasis on data security and privacy for health care providers. They are often designed to comply with regulations like HIPAA, ensuring that patient data is handled securely and confidentially by authorized providers.
Efficiency and Cost-Effectiveness
EHRs can improve the efficiency of healthcare services, reducing the time and cost associated with managing paper records. This can lead to cost savings and patient satisfaction for healthcare providers and patients.
Patient Empowerment
EHRs encourage patient participation in their own care. With features like patient portals, patients have easy and direct access to their health information, which can improve their understanding and engagement in their own medical and clinical data, health and treatment.
Key Points:
- EHRs enhance patient care by providing a more comprehensive health overview.
- They prioritize data security and privacy.
- EHRs increase efficiency and cost-effectiveness in healthcare.
- EHRs empower patients by providing easier access to their health information.

The Challenges of Implementing EHR
Technical and Financial Barriers
Implementing EHR systems in healthcare organization can be costly and technically challenging, especially for smaller practices. The cost of EHR software, hardware, and training different healthcare providers can be significant.
Resistance to Change
Change is hard, and the shift from EMR to the EHR system is no exception. Some healthcare providers might resist the change due to the comfort with existing systems or concerns about new technology.
Data Migration and Integration Issues
Transferring existing patient medical records from electronic health record to a new EHR system can be a complex process. Ensuring that data is accurately and effectively integrated is crucial.
Ensuring Compliance and Security
EHR systems must comply with various regulations, which can be a complex process. Ensuring the security of patient data in electronic medical record in a digital format is also a significant concern in the electronic medical records in practice.
Key Points:
- Implementing EHR systems can present financial and technical challenges.
- Resistance to change among healthcare providers can hinder EHR adoption.
- Data migration and integration into EHR systems can be complex.
- Compliance with regulations and ensuring data security are critical considerations.

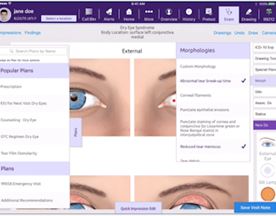
Software Tools for Managing EHR and EMR
Cerner
Known for its powerful EHR system, Cerner is widely used in hospitals and healthcare systems for its comprehensive data management and interoperability capabilities.
Epic
Epic is a leader in EHR technology, offering a robust platform that supports a wide range of healthcare operations, known for its user-friendly interface and scalability.
Meditech
Meditech provides versatile EHR solutions, catering to various healthcare environments, from small practices to large health systems.

Conclusion
Embracing the Digital Transformation in Healthcare
The shift in electronic health record, from EMR to EHR is a vital part of the digital transformation in the healthcare industry. It’s not just a change in health information technology though; it’s a change in the way healthcare is delivered and experienced.
The Future of Healthcare
With both population health management and the continuous advancement of technology, the potential for EHR systems to further improve healthcare delivery is enormous. We’re talking about things like integrating artificial intelligence with medical data for better diagnostics, using big data for more personalized treatment, and even linking wearable tech to EHRs for real-time health monitoring.
The Role of Patients and Providers
Both healthcare providers and patients play a crucial role in this transformation. Providers need to embrace these changes and invest in the necessary technology and training for patient support. Patients, on the other hand, need to be proactive in using the information management tools made available to them to engage in their health care. The patient has complete control and ownership of their own medical data.
Final Thoughts
The journey from EMR to EHR has been a significant one, and it’s far from over. As we continue to navigate this digital landscape, the focus of health organization should always be on improving healthcare outcomes, enhancing patient experiences, and making healthcare more accessible and efficient.
Key Points:
- The shift to EHR is a key part of the digital transformation in healthcare.
- Future advancements in EHR technology hold great potential for improving healthcare.
- Both healthcare providers and patients have crucial roles to play in this transformation.
- The ultimate goal of EHR adoption is to enhance healthcare delivery and patient experience.

Frequently Asked Questions
What is the main difference between EMR and EHR?
- EMRs are digital versions of paper charts within a single practice, while EHRs offer a comprehensive, shareable record across different healthcare settings.
Why are EHRs considered better than EMRs?
- EHRs provide a more holistic view of a patient’s health, facilitate better care coordination, and empower patients with access to their health information.
Can EHRs reduce medical errors?
- Yes, by providing comprehensive and accessible patient information, EHRs can help reduce medical errors.
How do EHRs impact patient privacy?
- EHRs are designed with strong data security and privacy protections in compliance with regulations like HIPAA.
Are EHRs expensive to implement?
- The initial cost can be high, especially for smaller practices, but they can lead to long-term savings and efficiency gains.
Do patients have access to their EHR?
- Yes, many EHR systems include patient portals for easy access to health information.
How do EHRs affect small medical practices?
- While beneficial, the cost and technical challenges of EHR implementation can be significant for small practices.
Can EHRs integrate with other digital health tools?
- Yes, EHRs are increasingly integrating with other digital health tools for comprehensive healthcare management.
How do healthcare providers ensure the security of EHRs?
- Providers must adhere to strict data security and privacy standards and regularly update their systems to protect patient data.